Never Use Alone hotline dial 877-696-1996. An operator will stay with you while you use, and call emergency services if needed.
Introduction
Data are a critical tool for understanding how opioid use is impacting our local community. Tompkins Whole Health tracks and publishes indicators related to opioid use within Tompkins County from a number of sources in an effort to provide the public as well as policy makers with information that is relevant and of interest. The data presented show the scale and scope of the crisis in Tompkins County.
On This Page
- Substance Use in Tompkins County
- Monthly 911 Calls for Overdose/ Poisoning received by TC (TC DoER)
- Unintentional Fatal Overdose Demographics (Tompkins County Medical Examiner)
- Drug Related Deaths (Tompkins County Medical Examiner)
- Opioid Quarterly Reports, Opioid OD deaths and opioid-related visits to an emergency department (ED). (NYSDOH)
- NYSDOH Opioid Dashboard
- Naloxone (Narcan®)
- Opioid Resources
Substance Use Data
Calls to 911 for Overdose Emergency
All calls that come into Tompkins County's 9-1-1 center are coded based on the type of the emergency. The code (called a Nature Code) informs the dispatcher on whether to assign the emergency to police, fire, or EMS.
When the 9-1-1 dispatcher receives a call for medical assistance, they will ask the caller certain key questions to ascertain if the cause might be drug induced based on protocols established by the department’s emergency medical dispatch program. Sometimes the cause is known by the caller, and other times the dispatcher makes the coding decision based on answers to their questions and other circumstances, and years of experience.
Total number of 9-1-1 calls per month that are C.A.D. coded as "Overdose/Poisoning," 2019-present. Computer Aided Dispatch (CAD) calls, Nature Code for “Overdoses/Poisoning.” Source: Tompkins County Department of Emergency Response (DoER).
Data source: TC Department of Emergency Response (DoER).
Unintentional fatal overdoses: demographic profile.
Like many communities, Tompkins County has experienced an increase in unintentional overdose deaths. When reviewing these datasets it is important to always remember that they represent individuals who are sons and daughters, families and friends whose lives have been interrupted or tragically ended, in some cases without warning.
The graphs below provide demographic information about the 100 people who died in Tompkins County from accidental drug overdose from 2019-2023. The larger sample size provided by totaling across five years increases the confidentiality of the individuals, and the confidence in how the data is interpreted.
“Unintentional Fatal Overdoses” includes those for which the “Manner of Death” is classified as an accident and substances identified in a toxicology screening are ruled as the immediate cause of death.
The US Census data (American Community Survey 2022 5-year estimates) compare the demographics of the deceased with the county population as a whole.
Drug Related Deaths
The deaths in this dataset may include overdose deaths due to pharmaceutically and illicitly produced, naturally occurring, semi-synthetic, and synthetic drugs. These deaths may not be attributed to an overdose.
“Drug Related Deaths” includes all deaths in which drugs are involved. In these cases, the immediate cause of death is not or not solely drugs, and drugs are often listed under “Other significant contributions.” These also include those in which the manner of death is not ruled as an accident.
NYS Opioid Quarterly Report
In accordance with the recommendations of the New York State Heroin and Opioid Task Force and 2016 legislation, the NYSDOH provides quarterly reports with opioid overdose information (deaths, emergency department (ED) visits, and hospitalizations) by county. Please note that the data presented in these are considered preliminary by the NYSDOH and should be used and interpreted with caution. Subsequent quarterly reports may contain figures which differ from a previous report due to additional confirmations, updates, and timing of data received. The reported cases are based on county of residence.
QUARTERLY RATE CALCULATION (person-years): [# events / (population X 0.25 years)] X 100,000.
Summary of Tompkins County data published October 2024
(Provisional data as of July 2024)
Overdose deaths
This dataset represents deaths from all opioids, including heroin, synthetics, and pharmaceuticals.
Emergency Department Visits and Hospitalizations
Emergency department visits and hospitalization rates help to show the extent of the opioid crisis in Tompkins County.
EMS Suspected Opioid Overdose Incidents
Full report on the NYSDOH website
- Complete current Quarterly Report dashboard for counties (July 2024 edition)
- Opioid Quarterly Report Archives (links to PDF reports and data files in Excel)
Naloxone (Narcan)
Naloxone is a lifesaving medication that can be administered to reverse an opioid overdose. Narcan is the most well-known brand of Naloxone and is used widely by emergency responders and members of the public, alike.
When naloxone is used at a scene by Emergency Medical Services (EMS), law enforcement, or registered overdose prevention programs, the incident is reported to New York State. The state compiles these incidents into quarterly reports, which are then available to the public.
Narcan Use
The trend of naloxone use is considered an indicator of the level of opioid use. The graph below is a visualization of these quarterly reports for Tompkins County (lower is better). You can see that overall naloxone use dipped in the first half of 2022, then did not fall again until Spring 2023. Numbers for Q2 2024 should be available October 2024
Narcan Training and Distribution
Many individuals carry Narcan with them so they are ready to act if they see someone who appears to be overcome by a drug overdose. Tompkins County Whole Health and its partners are working to distribute Narcan to more residents and train them in how to use it.
Across the state, the NYS Department of Health is setting up Opioid Overdose Prevention Program (OOPP) sites to distribute Narcan and train the public in its use. TCWH is a Registered OOPP, and members of the public may request Narcan at both our Brown Road and Green Street offices. A list of OOPP locations is below.
As part of its distribution program, TCWH is tracking the number of people trained and Narcan kits distributed by local OOPPs and reporting this information to the public. In the following graphs you can see how training dipped during the COVID-19 pandemic and has risen in the last three quarters of 2023.
The distribution of Narcan spray kits varies more from quarter to quarter since 2019, then increases at the end of 2023. Together, the graphs illustrate the increasing effort in Tompkins County to build a safety net across the community focused on reducing the number of deaths we experience due to drug overdoses.
NYS Opioid Data Dashboard:
- County (use the Select County dropdown menu to display the Tompkins dataset)
More information & resources: NYSDOH Opioid Data & Reports
Opioid Resources
In This Section
- How to lower the risk of opioid overdose
- Fentanyl
- Xylazine
- Drug Test Strips for Xylazine and Fentanyl
- NYS Drug Checking
- Naloxone (Narcan®)
- **How to give Narcan
- Local services and support
How to lower the risk of opioid overdose
- Never use alone. Use with others and take turns.
- Before using drugs, ask someone you trust to check on you regularly.
- If you are alone call the Never Use Alone hotline. Dial 1-877-696-1996. An operator will stay with you while you use, and call emergency services if needed.
- Test your drugs. Use test strips to test your drugs for Xylazine and Fentanyl. Drugs with one of these cut in can kill you.
- Always carry naloxone (Narcan®) with you.
- Go slow by taking small amounts, especially if you haven’t used for a while.
- Wait before taking more. Wait long enough to feel the effects of the drugs you took before taking more.
- Avoid mixing with alcohol or other drugs, especially drugs that make you sleepy.
- There is no safe dose of opioids.
Fentanyl
Fentanyl is a highly addictive synthetic substance that is added into illicit street drugs to increase consumption. It is also highly associated with risk of overdose death. The Tompkins County Health Department has issued a Health Alert warning of the high risk of the presence of Fentanyl locally in street drugs.
Harmful side effects include
- Sedation, confusion, drowsiness, dizziness, nausea, vomiting, urinary retention, pupillary constriction, and respiratory depression.
Signs of overdose include
- Stupor, changes in pupillary size (pinpoint size pupils), cold and clammy skin, cyanosis (blue discoloration of the skin), coma and respiratory failure leading to death.
Overdose prevention strategies
- Never use alone
- Use fentanyl test strips as a precaution
- Carry Narcan and be trained in its use
- Seek treatment and support
Xylazine
Xylazine (also called “tranq” or “tranq dope”) is a powerful non-opioid sedative or tranquilizer that is increasingly being found in the US illegal drug supply and linked to overdose deaths. Due to its impact on the opioid crisis, fentanyl mixed (adulterated) with xylazine has been declared an emerging threat by the White House’s Office of National Drug Control Policy. In one study, xylazine was found in almost 80% of drug samples that contained opioids (Maryland, 2021-2022). In another, xylazine was found in 31% of heroin and/or fentanyl overdose deaths (Philadelphia, 2019). [Source: CDC]
Symptoms and health risks of xylazine
- Sedation, difficulty breathing, dangerously low blood pressure, slowed heart rate, wounds that can become infected, severe withdrawal symptoms, death.
Reduce the overdose and the harms of overdose
- Never use alone.
- Provide rescue breaths, especially for people who have used xylazine since xylazine causes breathing to slow down. Harm reduction experts also suggest rolling individuals on their side, into the recovery position.
- Carry naloxone and learn how to use it. Because xylazine is often mixed with opioids like fentanyl, naloxone should be given in response to a suspected overdose to reverse any possible opioid effects. Importantly, naloxone will not reverse effects of xylazine. In the event of an overdose, call 911 for additional medical treatment.
- Reduce injection-related risks by using sterile injection equipment, rotating injection sites, allowing skin veins time to heal before another use, and taking drugs in other ways besides injection.
- Test drugs before using. There are commercially available test strips to test for the presence of xylazine in a sample of drugs. Test strips are available free of cost at a variety of local programs (see "Local services and support" section below).
[Top of Resources Section] | [Top of Page]
Test Strips for fentanyl and xylazine
- Fentanyl and Xylazine Test Strips can tell you if your drugs contain the synthetic opioid Fentanyl or the non-opioid sedative Xylazine. Both are frequently found in street drugs. Xylazine is always cut in with fentanyl, so drugs that test positive for xylazine will also contain fentanyl.
- If used correctly, these test strips can help to prevent overdose deaths and, with other risk reduction practices, save your life.
- Fentanyl Test Strips are blue and marked with the letters “FYL”.
- Xylazine Test Strips are red and marked with the letters “XYL”.
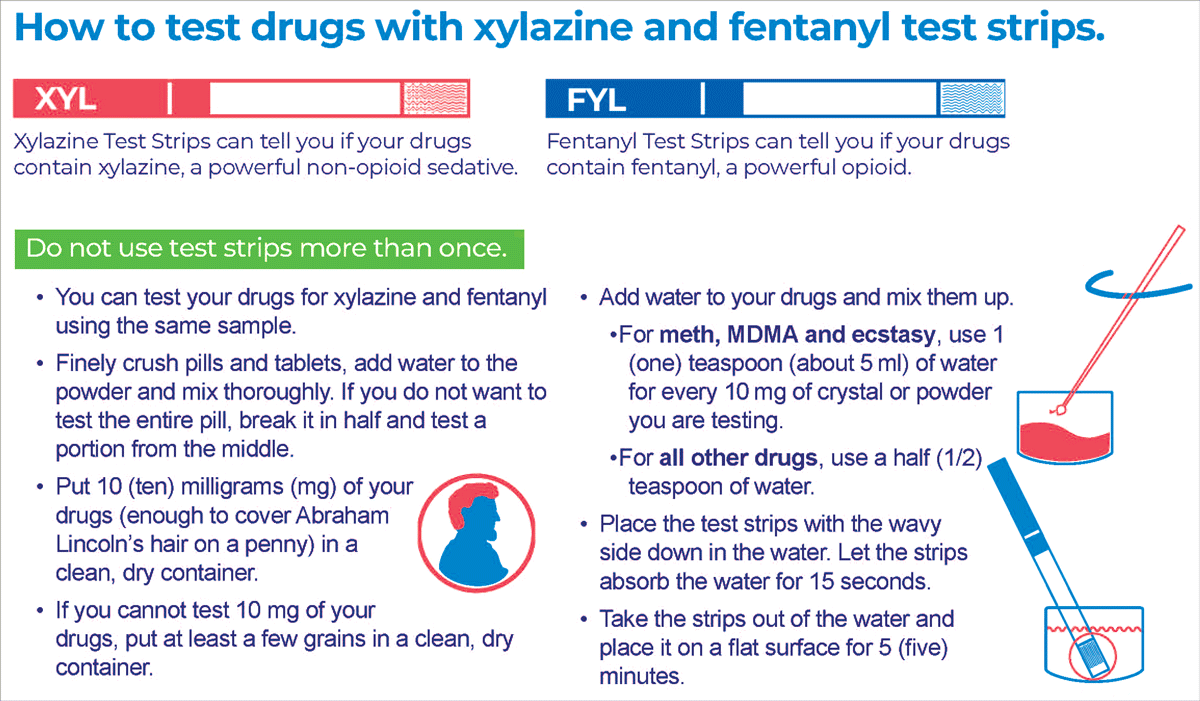
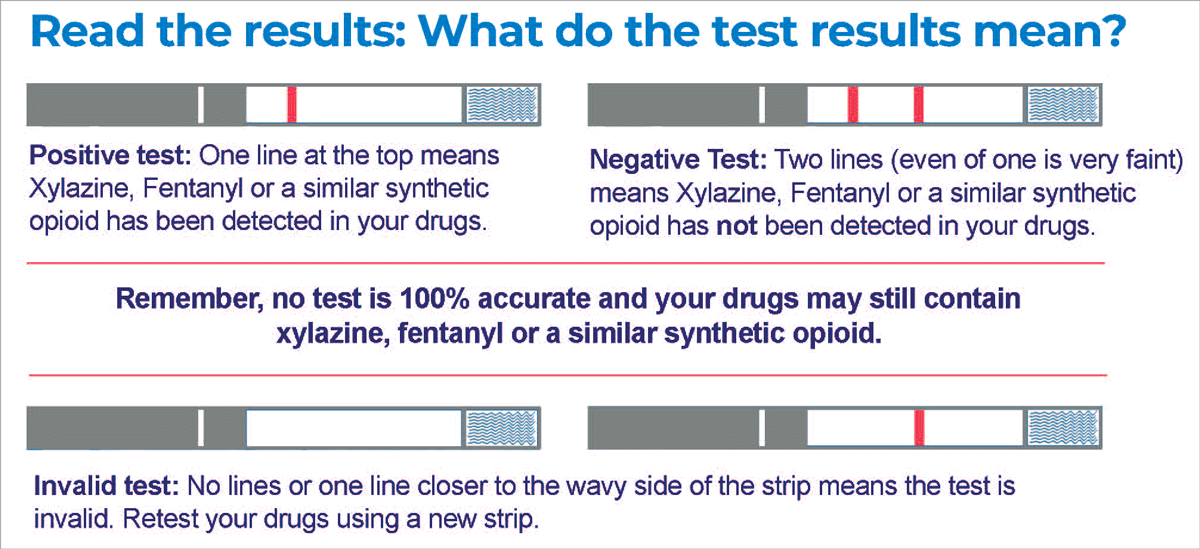
PDF version for how to use xylazine and fentanyl test strips.
NYS Drug Checking: Data on New York’s Unregulated Supply
New York's Drug Checking Service offers people who use drugs timely and detailed information on the contents of their drugs, helping them to make more informed decisions.
This service also shares information on New York's unregulated drug supply with harm reduction workers and clinicians to help them tailor the care they provide to people who use drugs, while informing advocacy, research, and policy.
The data page includes: Total samples, Monthly samples, Expected drugs, Expected vs. actual drug, Monthly trends, Noteworthy drug trends. The page also links to FAQs on drug checking, Drug Dictionary, Alerts, Resources.
Opioid Overdose Prevention Program (NYS OOP)
[Top of Resources Section] | [Top of Page]
Naloxone (Narcan®)
Naloxone (Narcan®) is a medication that can reverse the effects of an overdose from opioids, including fentanyl, heroin, and opioid-based pain killers. It is a tool that community members can use in emergency situations where opioid overdose occurs, providing a chance for individuals to receive further medical care and treatment.
Using Narcan
Used correctly, naloxone can reverse an opioid overdose. When Narcan is administered, it attaches to receptors in the brain and blocks opioids from having their usual effects. This helps to rapidly reverse an overdose by restoring normal breathing and providing an opportunity for medical assistance. There is no safety risk associated with naloxone.
How to Give Narcan:
- Call 9-1-1
- Carefully remove Narcan from packaging
- Hold the nasal spray with your thumb on the plunger
- Tilt the individuals’ head back
- Place the tip of the nasal spray in either nostril of the person experiencing an overdose, firmly press the plunger and release the entire dose of medication.
- Wait 2-3 minutes while checking for responsiveness
- If there is no response, give additional dose, switching nostrils, until help arrives.




Click here to open a 5-step guide for giving naloxone nasal spray.
Remember to always DIAL 9-1-1 FIRST. (Click here for a PDF.)
Watch this 30-second video for a quick "Naloxone/Narcan How-To" (30 seconds).
The video below shows you the signs of an overdose and how to respond and take the steps to prevent opioid overdose.
For additional information on how to use Naloxone (Narcan®), dial 2-1-1 for information about where you can get trained on how to use Naloxone (Narcan®) in our community.
Carry a Narcan kit with you
Opioid Overdose Prevention Programs (OOPPs) are organizations that provide individuals with training and a FREE Narcan kit to carry and dispense this potentially life-saving medication. OOPPs are registered by NYS Department of Health.
FREE Narcan kits are available at one of the local registered OOPP community agencies listed below.
- TC Whole Health, 201 E. Green St., Ithaca (downtown), and 55 Brown Rd., Ithaca (northeast).
- Cayuga Addiction Recovery Services (CARS), 334 W. MLK/State St. Ithaca, 607-273-5500, ext. 5811.
- Cayuga Health Emergency Department, 101 Dates Dr., Ithaca
- REACH Medical, 1001 W. Seneca St., (First Floor), Ithaca
- Southern Tier AIDS Program (STAP), 314 W. MLK/State St., Ithaca. STAP also provides free Drug Checking services.
For additional options Dial 2-1-1 (1-877-211-8667) 24/7. Or text your Zip code to TXT211 (898211). Available M-F 9 AM to 4 PM
Pharmacy Standing Order:
A statewide pharmacy standing order allows anyone* to get naloxone (Narcan®) nasal spray at a pharmacy without a prescription in NYS. Ask for it at the pharmacy counter. Insurance covers up to $40 copay. If you don’t have insurance, you can buy naloxone at the pharmacy.
*Dispensing to adolescents under age 18 is at the discretion of the pharmacist.
[Top of Resources Section] | [Top of Page]
Local and regional services and support
Emergency
- Call 911 immediately if you or someone you know is having a medical emergency.
- Suicide Prevention and Crisis Service, Crisis Line, 9-8-8, offers free and confidential crisis counseling, available 24/7.
Prevention
- Southern Tier AIDS Program (STAP): provides comprehensive HIV/AIDS services in the Southern Tier of NY. They provide the Opioid Overdose Prevention Program, which provides individuals with training, a Naloxone kit, and a prescription to be able to carry and dispense this potentially life-saving medication.
- Mental Health Association in Tompkins County, home page, was established in 1954, to address mental health needs in the Ithaca community.
- The Jenkins Center for Hope and Recovery is a drop-in center for those who use or have used mental health services. The Jenkins Center provides a safe environment where mental health consumers can relax, have fun with peers, and share information and support.
- The New York State Office of Addiction Services and Supports hosts “Project COPE”, a website which promotes overdose prevention and harm reduction education in New York State. The goal of this initiative is to empower people to learn how to prevent overdoses and save lives in their community.
- Additional resources for prevention services: NYS AIDS Institute Provider Directory
Using
- Sharps Collection and Disposal Sites in Tompkins County
- Never Use Alone hotline. Dial 1-877-696-1996. An operator will stay with you while you use, and call emergency services if needed.
- Test strips for Fentanyl and test strips for xylazine are available for free at the Southern Tier AIDS Program, REACH Medical, Cayuga Addiction Recovery Services, and Tompkins County Whole Health's office at 201 E. Green St.
- Narcan, fentanyl testing strips and xylazine testing strips can be ordered free of cost and delivered to your home via NYS OASAS. Complete the order form online at: oasas.ny.gov/harm-reduction.
- MATTERS facilitates rapid referrals to outpatient treatment for opioid and substance use disorders. Referrals are submitted online 24/7, 365 days a year by participating referral sites throughout NYS. Individuals may request test strips through the MATTERS website. Find them at mattersnetwork.org. Get the MATTERS Network mobile app on the App Store or Google Play.
- Community-based support groups are available for individuals to help navigate your personal recovery, as well as for friends and families affected by their loved one’s substance use.
Treatment
- Cayuga Addiction Recovery Services (CARS) offers intensive residential and out-patient treatment services, including Medication Assisted Treatment (MAT). CARS offers Open Access Monday thru Thursday from 8:30 a.m.–4:00 p.m. Clients need only to bring an insurance card, if they have one. 607-273-5500.
- REACH Medical provides medical and behavioral services, including MAT. The REACH Project is a non-profit operating as a low threshold, harm reduction medical practice in Ithaca. Reach Medical offers a wide range of services including: opioid replacement therapy, medical cannabis certification, Hep C treatment, primary care and behavioral services, in a stigma-free, inclusive setting. 607-273-7000. REACH Project Facebook page.
- NYS Office of Addiction Services & Support (OASAS): Treatment Finder
- About Medication Assisted Treatment (MAT)
Recovery
- Ithaca Community Recovery, is a non-profit organization that provides a meeting and activity space for Ithaca’s recovering community. They host a variety of meetings, including Alcoholics Anonymous, Al-Anon Meetings, Narcotics Anonymous, and more. Go to their website for meeting schedules.
- Mental Health Association in Tompkins County was established in 1954 to address mental health needs in the Ithaca community.
- The Jenkins Center for Hope and Recovery is a drop-in center for those who use or have used mental health services. The Jenkins Center provides a safe environment where mental health consumers can relax, have fun with peers, and share information and support.
Suicide Prevention
- Suicide Prevention and Crisis Service, offers free and confidential crisis counseling. The Crisis Line is available 24/7 at 9-8-8.
- Tompkins County Suicide Prevention Coalition.
- The Sophie Fund, Inc., a nonprofit charitable corporation established in 2017 to support mental health initiatives aiding young people in greater Ithaca and Tompkins County. It supports programs and projects; raises awareness and fights the stigma around mental illness and treatment; advances a “zero suicide” ethos in the community; and serves as a community advocate for young people struggling with mental illness.
National
- SAMHSA National Helpline FindTreatment.SAMHSA.gov/, 1-800-662-4357 (HELP). The Helpline provides free and confidential information in English and Spanish for individuals and family members facing substance abuse and mental health issues. 24 hours a day, 7 days a week. The website also has a location finder for the nearest treatment services based on the zip code entered.
- SAMHSA Resources for Families Coping with Mental and Substance Use Disorders

